What is Heart Disease ?
Heart disease is an umbrella term for a number of different diseases which affect the heart. The most common heart diseases are:
Coronary heart disease, a disease of the heart itself caused by the accumulation of atheromatous plaques within the walls of the arteries that supply the myocardium .
Ischaemic heart disease, another disease of the heart itself, characterized by reduced blood supply to the organ.
Cardiovascular disease, a sub-umbrella term for a number of diseases that affect the heart itself and/or the blood vessel system, especially the veins and arteries leading to and from the heart. Research on disease dimorphism suggests that women who suffer with cardiovascular disease usually suffer from forms that affect the blood vessels while men usually suffer from forms that affect the heart muscle itself. Known or associated causes of cardiovascular disease include diabetes mellitus, hypertension, hyperhomocysteinemia and hypercholesterolemia.
Pulmonary heart disease, a failure of the right side of the heart, not a good thing folks.
Hereditary heart disease, heart disease caused by unavoidable genetic factors since birth.
Hypertensive heart disease, heart disease caused by high blood pressure, especially localised high blood pressure .
Inflammatory heart disease, heart disease that involves inflammation of the heart muscle and/or the tissue surrounding it.
Valvular heart disease, heart disease that affects the valves of the heart.
Coronary Heart Disease
Coronary heart disease (CHD), also called coronary artery disease (CAD), ischaemic heart disease, and atherosclerotic heart disease, is the end result of the accumulation of atheromatous plaques within the walls of the arteries that supply the myocardium (the muscle of the heart). While the symptoms and signs of coronary heart disease are noted in the advanced state of disease, most individuals with coronary heart disease show no evidence of disease for decades as the disease progresses before the first onset of symptoms, often a "sudden" heart attack, finally arise. After decades of progression, some of these atheromatous plaques may rupture and (along with the activation of the blood clotting system) start limiting blood flow to the heart muscle. The disease is the most common cause of sudden death, and is also the most common reason for death of men and women over 65 years of age.
Atherosclerotic heart disease can be thought of as a wide spectrum of disease of the heart. At one end of the spectrum is the asymptomatic individual with atheromatous streaks within the walls of the coronary arteries (the arteries of the heart). These streaks represent the early stage of atherosclerotic heart disease and do not obstruct the flow of blood. A coronary angiogram performed during this stage of disease may not show any evidence of coronary artery disease, because the lumen of the coronary artery has not decreased in calibre.
Over a period of many years, these streaks increase in thickness. While the atheromatous plaques initially expand into the walls of the arteries, eventually they will expand into the lumen of the vessel, affecting the flow of blood through the arteries. While it was originally believed that the growth of atheromatous plaques was a slow, gradual process, recent evidence suggests that the gradual buildup of plaque may be complemented by small plaque ruptures which cause the sudden increase in the plaque burden due to accumulation of thrombus material. This is a common misconception many have had.
Atheromatous plaques that cause obstruction of less than 70 percent of the diameter of the vessel rarely cause symptoms of obstructive coronary artery disease. As the plaques grow in thickness and obstruct more than 70 percent of the diameter of the vessel, the individual develops symptoms of obstructive coronary artery disease. At this stage of the disease process, the patient can be said to have ischemic heart disease. The symptoms of ischemic heart disease are often first noted during times of increased workload of the heart. For instance, the first symptoms include exertional angina or decreased exercise tolerance.
As the degree of coronary artery disease progresses, there may be near-complete obstruction of the lumen of the coronary artery, severely restricting the flow of oxygen-carrying blood to the myocardium. Individuals with this degree of coronary heart disease typically have suffered from one or more myocardial infarctions (heart attacks), and may have signs and symptoms of chronic coronary ischemia, including symptoms of angina at rest and flash pulmonary edema.
A distinction should be made between myocardial ischemia and myocardial infarction. Ischemia means that the amount of oxygen supplied to the tissue is inadequate to supply the needs of the tissue. When the myocardium becomes ischemic, it does not function optimally. When large areas of the myocardium becomes ischemic, there can be impairment in the relaxation and contraction of the myocardium. If the blood flow to the tissue is improved, myocardial ischemia can be reversed. Infarction means that the tissue has undergone irreversible death due to lack of sufficient oxygen-rich blood.
An individual may develop a rupture of an atheromatous plaque at any stage of the spectrum of coronary heart disease. The acute rupture of a plaque may lead to an acute myocardial infarction (heart attack).
Blood Flow to Heart
Limitation of blood flow to the heart causes ischemia (cell starvation secondary to a lack of oxygen) of the myocardial cells. When myocardial cells die from lack of oxygen, this is called a myocardial infarction (commonly called a heart attack). It leads to heart muscle damage, heart muscle death and later scarring without heart muscle regrowth.
Myocardial infarction usually results from the sudden occlusion of a coronary artery when a plaque ruptures, activating the clotting system and atheroma-clot interaction fills the lumen of the artery to the point of sudden closure. The typical narrowing of the lumen of the heart artery before sudden closure is typically 20%, according to clinical research completed in the late 1990s and using IVUS examinations within 6 months prior to a heart attack. High grade stenoses as such exceeding 75% blockage, such as detected by stress testing, were found to be responsible for only 14% of acute heart attacks the rest being due to plaque rupture/ spasm. The events leading up to plaque rupture are only partially understood. Myocardial infarction is also caused, far less commonly, by spasm of the artery wall occluding the lumen, a condition also associated with atheromatous plaque and CHD.
CHD is associated with smoking, obesity, hypertension and a chronic sub-clinical lack of vitamin C. A family history of CHD is one of the strongest predictors of CHD. Screening for CHD includes evaluating homocysteine levels, high-density and low-density lipoprotein (cholesterol) levels and triglyceride levels.
Angina that occurs regularly with activity, upon awakening, or at other predictable times is termed stable angina and is associated with high grade narrowings of the heart arteries. The symptoms of angina are often treated with nitrate preparations such as nitroglycerin, which come in short-acting and long-acting forms, and may be administered transdermally, sublingually or orally. Many other more effective treatments, especially of the underlying atheromatous disease, have been developed.
Angina that changes in intensity, character or frequency is termed unstable. Unstable angina may precede myocardial infarction, and requires urgent medical attention. It is treated with morphine, oxygen, intravenous nitroglycerin, and aspirin. Interventional procedures such as angioplasty may be done.
Heart Disease Risk factors
The following are confirmed independent risk factors for the development of CAD, in order of decreasing importance:
*Hypercholesterolemia (specifically, serum LDL concentrations)
*Smoking
*Hypertension (high systolic pressure seems to be most significant in this regard)
* Hyperglycemia (due to diabetes mellitus or otherwise)
Hereditary differences in such diverse aspects as lipoprotein structure and that of their associated receptors, homocysteine processing/metabolism, etc.
Significant, but indirect risk factors include:
*Lack of exercise
*Stress
*Diet rich in saturated fats
*Diet low in antioxidants
*Obesity
*Men or Women over 65
Heart Disease Prevention
Coronary heart disease is the most common form of heart disease in the Western world. Prevention centers on the modifiable risk factors, which include decreasing cholesterol levels, addressing obesity and hypertension, avoiding a sedentary lifestyle, making healthy dietary choices, and stopping smoking. There is some evidence that lowering uric acid and homocysteine levels may contribute. In diabetes mellitus, there is little evidence that blood sugar control actually improves cardiac risk. Some recommend a diet rich in omega-3 fatty acids and vitamin C. The World Health Organization (WHO) recommends "low to moderate alcohol intake" to reduce risk of coronary heart disease.
An increasingly growing number of other physiological markers and homeostatic mechanisms are currently under scientific investigation. Among these markers are low density lipoprotein and asymmetric dimethylarginine. Patients with CHD and those trying to prevent CHD are advised to avoid fats that are readily oxidized (e.g., saturated fats and trans-fats), limit carbohydrates and processed sugars to reduce production of Low density lipoproteins while increasing High density lipoproteins, keeping blood pressure normal, exercise and stop smoking. These measures limit the progression of the disease. Recent studies have shown that dramatic reduction in LDL levels can cause mild regression of coronary heart disease.
Diet and Heart Disease
It has been suggested that coronary heart disease is partially reversible using an intense dietary regime coupled with regular cardio exercise.
Vegetarian diet: Vegetarians have been shown to have a 24% reduced risk of dying of heart disease.
Cretan Mediterranean-style diet: The Seven Country Study found that Cretan men had exceptionally low death rates from heart disease, despite moderate to high intake of fat. The Cretan diet is similar to other traditional Mediterranean diets: consisting mostly of olive oil, bread, abundant fruit and vegetables, a moderate amount of wine and fat-rich animal products such as lamb, sausage and goat cheese. However, the Cretan diet consisted of less fish and wine consumption than some other Mediterranean-style diets, such as the diet in Corfu, another region of Greece, which had higher death rates.
The consumption of trans fat (commonly found in hydrogenated products such as margarine) has been shown to cause the development of endothelial dysfunction, a precursor to atherosclerosis.
Aspirin can reduce the incidence of cardiovascular events. The U.S. Preventive Services Task Force 'strongly recommends that clinicians discuss aspirin chemoprevention with adults who are at increased risk for coronary heart disease'. The Task Force defines increased risk as 'Men older than 40 years of age, postmenopausal women, and younger persons with risk factors for coronary heart disease (for example, hypertension, diabetes, or smoking) are at increased risk for heart disease and may wish to consider aspirin therapy'. More specifically, high-risk persons are 'those with a 5-year risk ≥ 3%'. A risk calculator is available.
Regarding healthy premenopausal women, the more recent Women's Health Study randomized controlled trial found no insignficant benefit from aspirin in the reduction of cardiac events; however there was a signficant reduction in stroke. Subgroup analysis showed that all benefit was confined to women over 65 years old. In spite of the insignficant benefit for women < 65 years old, recent practice guidelines by the American Heart Association recommend to 'consider' aspirin in 'healthy women' <65 years of age 'when benefit for ischemic stroke prevention is likely to outweigh adverse effects of therapy'.
Secondary prevention is preventing further sequelae of already established disease. Regarding coronary heart disease, this can mean risk factor management that is carried out during cardiac rehabilitation, a 4-phase process beginning in hospital after MI, angioplasty or heart surgery and continuing for a minimum of three months. Exercise is a main component of cardiac rehabilitation along with diet, smoking cessation, and blood pressure and cholesterol management .
Cardiovascular Disease
Cardiovascular disease refers to the class of diseases that involve the heart and/or blood vessels (arteries and veins). While the term technically refers to any disease that affects the cardiovascular system, it is usually used to refer to those related to atherosclerosis (arterial disease).
These conditions have similar causes, mechanisms, and treatments. In practice, cardiovascular disease is treated by cardiologists, thoracic surgeons, vascular surgeons, neurologists, and interventional radiologists, depending on the organ system that is being treated. There is considerable overlap in the specialities, and it is common for certain procedures to be performed by different types of specialists in the same hospital.
Most Western countries face high and increasing rates of cardiovascular disease. Each year, heart disease kills more Americans than cancer. Diseases of the heart alone caused 30% of all deaths, with other diseases of the cardiovascular system causing substantial further death and disability. It is the number 1 cause of death and disability in the United States and most European countries. A large histological study (PDAY) showed vascular injury accumulates from adolescence, making primary prevention efforts necessary from childhood. By the time that heart problems are detected, the underlying cause (atherosclerosis) is usually quite advanced, having progressed for decades. There is therefore increased emphasis on preventing atherosclerosis by modifying risk factors, such as healthy eating, exercise and avoidance of smoking.
There are many risk factors which associate with (but are not all causes of) various forms of cardiovascular disease. These include the following:
*Age Gender, men under age 64 are much more likely to die of coronary heart disease than women, although the gender difference declines with age. (The gender difference is less pronounced in blacks than in whites, but it is still significant )
*Absence of key nutritional elements, such as omega-3 fats and polyphenol antioxidants
*Diabetes mellitus
*Hypercholesterolemia (elevated cholesterol levels) and abnormal lipoprotein particle profile (cholesterol subtypes)
*Elevated Heart Rate
*Tobacco smoking
*Higher fibrinogen and PAI-1 blood concentrations
*Elevated homocysteine, or even upper half of normal
*Elevated blood levels of asymmetric dimethylarginine
*High blood pressure
*Exposure to high levels of environmental noise
*Obesity, especially central or male-type obesity; apart from being linked to diabetes, this form of obesity independently increases cardiovascular risk, presumedly by inducing an inflammatory and procoagulant state
*Insulin resistance, especially when excess food calories are ingested
*Genetic factors/Family history of cardiovascular disease
*Physical inactivity/ Sedentary lifestyle
*Depression
*Stress
Although men have a higher rate of cardiovascular disease than women, it is also the number one health problem for women in industrialized countries. After menopause, the risk for women approaches that of men. Hormone replacement therapy alleviates a number of post-menopausal problems, but appears to increase the risk of cardiovascular disease.
Attempts to prevent cardiovascular disease are more effective when they remove and prevent causes, and they often take the form of modifying risk factors. Some factors, such as sex (male or female), age, and family history, cannot be modified. Smoking cessation (or abstinence) is one of the most effective and easily modifiable changes. Regular cardiovascular exercise (aerobic exercise) complements the healthful eating habits.
According to the American Heart Association, build up of plaque on the arteries (atherosclerosis), partly as a result of high cholesterol and fat diet, is a leading cause for cardiovascular diseases. The combination of healthy diet and exercise is a means to improve serum cholesterol levels and reduce risks of cardiovascular diseases; if not, a physician may prescribe "cholesterol-lowering" drugs, such as the statins. These medications have additional protective benefits aside from their lipoprotein profile improvement. Aspirin may also be prescribed, as it has been shown to decrease the clot formation that may lead to myocardial infarctions and strokes; it is routinely prescribed for patients with one or more cardiovascular risk factors.
One possible way to decrease risk of cardiovascular disease is keep your total cholesterol below 150. In the Framingham Heart Study, those with total cholesterol below 150 only very rarely got coronary heart disease.
Eating oily fish at least twice a week may help reduce the risk of sudden death and arrhythmias. A 2005 review of 97 clinical trials by Studer et al. noted that omega-3 fats gave lower risk ratios than did statins. Olive oil is said to have benefits. Studies of individual heart cells showed that fatty acids blocked excessive sodium and calcium currents in the heart, which could otherwise cause dangerous, unpredictable changes in its rhythm.
Interestingly, although cardiovascular is the number one cause of death for individuals in modern society, a majority of young people are unconcerned about their risk for development of this disease. Atherosclerosis is a process that develops over decades and is often silent until an acute event (heart attack) develops in later life. Population based studies in the youth show that the precursors of heart disease start in adolescence. The process of atherosclerosis evolves over decades, and begins as early as childhood. The Pathobiological Determinants of Atherosclerosis in Youth Study demonstrated that intimal lesions appear in all the aortas and more than half of the right coronary arteries of youths aged 15–19 years. However, most adolescents are more concerned about other risks such as HIV, accidents, and cancer than cardiovascular disease. This is extremely important considering that 1 in 3 people will die from complications attributable to atherosclerosis. In order to stem the tide of cardiovascular disease, primary prevention is needed. Primary prevention starts with education and awareness that cardiovascular disease poses the greatest threat and measures to prevent or reverse this disease must be taken.
Treatment of cardiovascular disease depends on the specific form of the disease in each patient, but effective treatment always includes preventive lifestyle changes discussed above. Medications, such as blood pressure reducing medications, aspirin and the statin cholesterol-lowering drugs may be helpful. In some circumstances, surgery or angioplasty may be warranted to reopen, repair, or replace damaged blood vessels.
The causes, prevention, and/or treatment of all forms of cardiovascular disease are active fields of biomedical research, with hundreds of scientific studies being published on a weekly basis. A fairly recent emphasis is on the link between low-grade inflammation that hallmarks atherosclerosis and its possible interventions. C-reactive protein (CRP) is an inflammatory marker that may be present in increased levels in the blood in patients at risk for cardiovascular disease. Its exact role in predicting disease is the subject of debate.
Some areas currently being researched include possible links between infection with Chlamydia pneumoniae and coronary artery disease. The Chlamydia link has become less plausible with the absence of improvement after antibiotic use .
Pulmonary heart disease - Cor pulmonale is a medical term used to describe a change in structure and function of the right ventricle of the heart as a result of a respiratory disorder. RVH (right ventricular hypertrophy) is the predominant change in chronic cor pulmonale, however in acute cases dilation dominates. Both hypertrophy and dilation are the result of increased right ventricular pressure. Dilation is essentially a stretching of the ventricle, the immediate result of increasing the pressure in an elastic container. Ventricular hypertrophy is an adaptive response to a long-term increase in pressure. Additional muscle grows to allow for the increased force in contraction required to move the blood against greater resistance. To be classified as cor pulmonale, the cause must originate in the pulmonary circulation. Vascular remodelling of the pulmonary circulation as a result of tissue damage (causes including disease, hypoxic injury, chemical agents, etc.) or chronic hypoxic vasoconstriction are two major causes. RVH due to a systemic defect is not classified as cor pulmonale. Left untreated, cor pulmonale can lead to right-heart failure and death.
Pulmonary heart diseaseTreatment - Elimination of the cause is the most important intervention. In pulmonary embolism, thrombolysis (enzymatic dissolution of the blood clot) is advocated if there is dysfunction of the right ventricle. In COPD, long-term oxygen therapy may improve cor pulmonale.
Cor pulmonale may lead to congestive heart failure (CHF), with worsening of respiration due to pulmonary edema, swelling of the legs due to peripheral edema and painful congestive hepatomegaly. This situation requires diuretics (to decrease strain on the heart), sometimes nitrates (to improve blood flow) and occasionally inotropes (to improve heart contractility). CHF is a negative prognostic indicator in cor pulmonale.
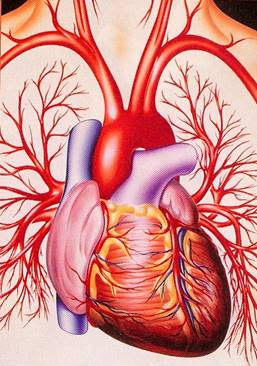
What is the Heart ?
The heart is a pear shaped, muscular organ in vertebrates, responsible for pumping blood through the blood vessels by repeated, rhythmic contractions, or a similar structure in annelids, mollusks, and arthropods. The term cardiac (as in cardiology) means "related to the heart" and comes from the Greek καρδία, kardia, for "heart." The heart is composed of cardiac muscle, an involuntary muscle tissue which is found only within this muscle.
The human embryonic heart begins beating approximately 21 days after conception, or five weeks after the last normal menstrual period (LMP), which is the date normally used to date pregnancy. The human heart begins beating at a rate near the mother’s, about 75-80 beats per minute (bpm). The embryonic heart rate (EHR) then accelerates linearly for the first month of beating, peaking at 165-185 bpm during the early 7th week, (early 9th week after the LMP). This acceleration is approximately 3.3 bpm per day, or about 10 bpm every three days, an increase of 100 bpm in the first month. There is no difference in male and female heart rates before birth
In the human body, the heart is normally situated to the left of the middle of the thorax, underneath the breastbone (see diagrams). The heart is usually felt to be on the left side because the left heart (left ventricle) is stronger (it pumps to all body parts). The left lung is smaller than the right lung because the heart occupies more of the left hemithorax. The heart is enclosed by a sac known as the pericardium and is surrounded by the lungs. The pericardium is a double membrane structure containing a serous fluid to reduce friction during heart contractions. The mediastinum, a subdivision of the thoracic cavity, is the name of the heart cavity.
The apex is the blunt point situated in an inferior (pointing down and left) direction. A stethoscope can be placed directly over the apex so that the beats can be counted. This physical location is between the sixth and seventh rib, just to the left of the sternum . In normal adults, the mass of the heart is 250-350 g (9-12 oz), or about three fourths the size of a clenched fist, but extremely diseased hearts can be up to 1000 g (2 lb) in mass due to hypertrophy. It consists of four chambers, the two upper atria (singular: atrium ) and the two lower ventricles. On the left is a picture of a fresh human heart which was removed from a 64-year-old British male.
The function of the right side of the heart (see right heart) is to collect deoxygenated blood, in the right atrium, from the body and pump it, via the right ventricle, into the lungs (pulmonary circulation) so that carbon dioxide can be dropped off and oxygen picked up (gas exchange). This happens through a passive process called diffusion. The left side (see left heart) collects oxygenated blood from the lungs into the left atrium. From the left atrium the blood moves to the left ventricle which pumps it out to the body. On both sides, the lower ventricles are thicker and stronger than the upper atria. The muscle wall surrounding the left ventricle is thicker than the wall surrounding the right ventricle due to the higher force needed to pump the blood through the systemic circulation.
If a person is encountered in cardiac arrest (no heartbeat), cardiopulmonary resuscitation (CPR) should be started, and help called. If an automated external defibrillator is available, this device may automatically administer defibrillation if this is indicated.
Heart cancer is an extremely rare form of cancer of the heart. Heart cancer is divided into primary tumors of the heart and secondary tumors of the heart. Most heart cancers are benign myxomas, fibromas, rhabdomyomas and hamartomas, although malignant sarcomas (such as angiosarcoma or cardiac sarcoma) have been known to occur. In a study of 12,487 autopsies performed in Hong Kong seven cardiac tumors were found, most of which were benign. However, cancer can also spread to heart from other parts of the body. In addition the heart can be affected by treatment for cancer in other parts of the body
A congenital heart defect (CHD) is a defect in the structure of the heart and great vessels of the newborn. Most heart defects either obstruct blood flow in the heart or vessels near it or cause blood to flow through the heart in an abnormal pattern, although other defects affecting heart rhythm (such as long QT syndrome) can also occur. Heart defects are among the most common birth defects, and are the leading cause of birth defect-related deaths.
Slightly less than 1% of all newborn infants have congenital heart disease. Eight defects are more common than all others and make up 80% of all congenital heart diseases, whereas the remaining 20% consist of many independently infrequent conditions or combinations of several defects. Ventricular septal defect (VSD) is generally considered to be the most common type of malformation, accounting for about 1/3 of all congenital heart defects.
The incidence is higher when a parent or a sibling has a heart defect (4-5%), in stillborns (3-4%), abortuses (10-25%), and premature infants (2%).
The number of adults with problems connected to a congenital heart defect is rising and is passing the number of children with congenital heart defects in most western countries. This group is called GUCH patients.
The cause of most congenital heart defects is unknown. Where a cause is known, it may be of a multifactorial origin and/or a result of genetic predisposition and environmental factors. Known genetic causes of heart disease includes chromosomal abnormalities such as trisomies 21, 13, and 18, as well as a range of newly recognised genetic point mutations, point deletions and other genetic abnormalities as seen in syndromes such as CATCH 22, familial ASD with heart block, Alagille syndrome, Noonan syndrome, and many more.
Known antenatal environmental factors include maternal infections (Rubella), drugs (alcohol, hydantoin, lithium and thalidomide) and maternal illness (diabetes mellitus, phenylketonuria, and systemic lupus erythematosus).
Symptoms and signs are related to the type and severity of the heart defects. Some children have no signs while others may exhibit shortness of breath, cyanosis, chest pain, syncope, sweating, heart murmur, respiratory infections, underdeveloping of limbs and muscles, poor feeding, or poor growth. Most defects cause a whispering sound, or murmur, as blood moves through the heart causing some of these symptoms. All of these symptoms occur at a young age of a child or infant which is typically found during a physical examination.
Heart rate is a term used to describe the frequency of the cardiac cycle. It is considered one of the four vital signs. Usually it is calculated as the number of contractions (heart beats) of the heart in one minute and expressed as "beats per minute" (bpm). See "Heart" for information on embryofetal heart rates. The heart beats up to 120 times per minute in childhood. When resting, the adult human heart beats at about 70 bpm (males) and 75 bpm (females), but this rate varies among people. However, the resting heart rate can be significantly lower in athletes. The infant/neonatal rate of heartbeat is around 130-150 bpm, the toddler's about 100–130 bpm, the older child's about 90–110 bpm, and the adolescent's about 80–100 bpm.
The pulse is the most straightforward way of measuring the heart rate, but it can be deceptive when some heart beats do not have much cardiac output. In these cases (as happens in some arrhythmias), the heart rate may be considerably higher than the pulse rate. Auscultation is also a method of heart rate measurement.
The heart contains two cardiac pacemakers that spontaneously cause the heart to beat. These can be controlled by the autonomic nervous system and circulating adrenaline. The vagus nerve (which is pneumogastric nerve or cranial nerve X) which governs heart rate can be controlled through breathing.
Measuring heart rate - The pulse rate (which in most people is identical to the heart rate) can be measured at any point on the body where an artery is close to the surface. Such places are wrist (radial artery), neck (carotid artery), elbow (brachial artery), and groin (femoral artery). The pulse can also be felt directly over the heart. NOTE: The thumb should never be used for measuring heart rate. Producing an electrocardiogram, or ECG (also abbreviated EKG), is one of the most precise methods of heart rate measurement. Continuous electrocardiographic monitoring of the heart is routinely done in many clinical settings, especially in critical care medicine. Commercial heart rate monitors are also available, consisting of a chest strap with electrodes. The signal is transmitted to a wrist receiver for display. Heart rate monitors allow accurate measurements to be taken continuously and can be used during exercise when manual measurement would be difficult or impossible (such as when the hands are being used). It is also common to find heart rate by listening, via a stethoscope, to the movement created by the heart as it contracts within the chest
Heart rate variability (HRV) is the variation of beat-to-beat intervals. A healthy heart has a large HRV, while decreased or absent variability may indicate cardiac disease. HRV also decreases with exercise-induced tachycardia. HRV has been the focus of increased research to use it as a physiological marker to classify different pathological disorders.
One aspect of heart rate variability can be used as a measurement of fitness, specifically the speed at which one's heart rate drops upon termination of vigorous exercise. The speed at which a person's heart rate returns to resting is considerably faster for a fit person than an unfit person. A drop of 20 beats in a minute is typical for a healthy person. A drop of less than 12 beats per minute after maximal exercise has been correlated with a significant increase in mortality
Maximum heart rate (also called MHR, or HRmax) is the maximum heart rate that a person should achieve during maximal physical exertion. Research indicates it is most closely linked to a person's age; a person's HRmax will decline as they age. Some research indicates the speed at which it declines over time is related to fitness—the more fit a person is, the more slowly it declines as they age.
HRmax is utilized frequently in the fitness industry, specifically during the calculation of target heart rate when prescribing a fitness regimen. A quick way to estimate MHR is to subtract your age from 220, but HRmax can vary significantly between same-aged individuals so direct measurement using a heart rate monitor (and with medical supervision or at least permission and advice) should be used by those seeking maximum safety and effectiveness in their training. People who have participated in sports and athletic activities in early years will have a higher MR than those less active as children.
Training Heart rates - (Warm up) — 50–60% of maximum heart rate: The easiest zone and probably the best zone for people just starting a fitness program. It can also be used as a warm up for more serious walkers. This zone has been shown to help decrease body fat, blood pressure and cholesterol. It also decreases the risk of degenerative diseases and has a low risk of injury. Fats are 85% of food energy burned in this zone.
Fitness Zone (Fat Burning) — 60–70% of maximum heart rate: This zone provides the same benefits as the healthy heart zone, but is more intense and burns more total food energy. The percent of food energy from fat is still 85%.
Aerobic Zone (Endurance Training) — 70–80% of maximum heart rate: The aerobic zone will improve your cardiovascular and respiratory system and increase the size and strength of your heart. This is the preferred zone if you are training for an endurance event. More food energy is burned with 50% from fat.
Anaerobic Zone (Performance Training) — 80–90% of maximum heart rate: Benefits of this zone include an improved FPRIVATE "TYPE=PICT;ALT=V_{\mathrm{O}_2 }" maximum (the highest amount of oxygen one can consume during exercise) and thus an improved cardio-respiratory system, and a higher lactate tolerance ability which means your endurance will improve and you'll be able to fight fatigue better. This is a high intensity zone burning more food energy, 15% from fat.
Red Line (Maximum Effort) — 90–100% of maximum heart rate: Although this zone burns the highest amount of food energy, it is very intense. Most people can only stay in this zone for short periods. You should only train in this zone if you have a very high fitness level and have been cleared by a physician to do so.
Recovery heart rate - The recovery heart rate is one that is taken several minutes after exercise. It is taken anywhere between 2–10 minutes after exercise. It is taken for 15 seconds, and is multiplied by four in order to calculate beats per minute (bpm). The goal is not to exceed 120 bpm.
Target heart rate (THR), or training heart rate, is a desired range of heart rate reached during aerobic exercise which enables one's heart and lungs to receive the most benefit from a workout. This theoretical range varies based on one's physical condition, age, and previous training. Below are two ways to calculate one's Target Heart Rate. In each of these methods, there is an element called "intensity" which is expressed as a percentage. THR can be calculated by using a range of 50%–85% intensity.
Heart rate reserve (HRR) is a term used to describe the difference between a person's maximum heart rate and predicted heart rate (or actual heart rate). Some methods of measurement of exercise intensity measure percentage of heart rate reserve. Additionally, as a person increases their cardiovascular fitness, their HRrest will drop, thus the heart rate reserve will increase. Percentage of HRR is equivalent to percentage of VO2reserve.
Heart rate abnormalities :
Tachycardia is a resting heart rate more than 100 beats per minute. This number can vary as smaller people and children have faster heart rates than adults.
Bradycardia is defined as a heart rate less than 60 beats per minute although it is seldom symptomatic until below 50 bpm. Trained athletes tend to have slow resting heart rates, and resting bradycardia in athletes should not be considered abnormal if the individual has no symptoms associated with it. Again, this number can vary as smaller people and children have faster heart rates than adults
In medicine, a person's pulse is the throbbing of their arteries as an effect of the heart beat. It can be felt at the neck, at the wrist and other places.
Pressure waves move through the blood vessels, which are pliable; these waves are not caused by the forward movement of the blood. When the heart contracts, blood is ejected into the aorta and the aorta stretches. At this point the wave of distention (pulse wave) is pronounced but relatively slow-moving (3 to 6 m/s). As it travels towards the peripheral blood vessels, it gradually diminishes and becomes faster. In the large arterial branches, its velocity is 7 to 10 m/s; in the small arteries, it is 15 to 35 m/s. The pressure pulse is transmitted 15 or more times more rapidly than the blood flow.
The term pulse is also used, although incorrectly, to denote the frequency of the heart beat, usually measured in beats per minute. In most people, the pulse is an accurate measure of heart rate. Under certain circumstances, including arrhythmias, some of the heart beats are ineffective and the aorta is not stretched enough to create a palpable pressure wave. The pulse is irregular and the heart rate can be (much) higher than the pulse rate. In this case, the heart rate should be determined by auscultation of the heart apex, in which case it is not the pulse. The pulse deficit (difference between heart beats and pulsations at the periphery) should be determined by simultaneous palpation at the radial artery and auscultation at the heart apex.
A normal pulse rate for a healthy adult, while resting, can range from 60 to 100 beats per minute (BPM). During sleep, this can drop to as low as 40 BPM; during strenuous exercise, it can rise as high as 200–220 BPM. Generally, pulse rates are higher in younger persons. A resting heart rate for an infant is as high as or higher than an adult's pulse rate during strenuous exercise.
Besides its rate, the pulse has other qualities which reflect the state of the cardiovascular system, such as its rhythm, fullness and the shape of the pulse wave. Certain diseases cause characteristic changes in these qualities. The absence of a pulse at the temple of the skull can be a sign of giant cell arteritis; absent or decreased pulses in the limbs may indicate peripheral artery occlusive disease.
Pulses are manually palpated with fingers or thumb. When palpating the carotid artery, the femoral artery or the brachial artery, the thumb may be used. However, the thumb has its own pulse which can interfere with detecting the patient's pulse at other points, where two or three fingers should be used. Fingers or thumb must be placed near an artery and pressed gently against a firm structure, usually a bone, in order to feel the pulse.
An alternative way of finding the pulse rate is by palpating or listening to the heartbeat. This is most commonly done with the examiner's palm or a through a stethoscope. Before the invention of the stethoscope examiners would press their ear directly to the chest.
Common pulse points :
radial pulse - located on the thumb side of the wrist (radial artery)
ulnar pulse - located on the little finger side of the wrist (ulnar artery)
carotid pulse - located in the neck (carotid artery). The carotid artery should be palpated gently. Stimulating its baroreceptors with vigorous palpitation can provoke severe bradycardia or even stop the heart in some sensitive persons. Also, a person's two carotid arteries should not be palpated at the same time, to avoid a risk of fainting or brain ischemia.
brachial pulse - located between the biceps and triceps, on the medial side of the elbow cavity; frequently used in place of carotid pulse in infants (brachial artery)
femoral pulse - located in the thigh (femoral artery)
popliteal pulse - located behind the knee in the popliteal fossa, found by holding the bent knee. The patient bends the knee at approximately 120°, and the physician holds it in both hands to find the popliteal artery in the pit behind the knee.
dorsalis pedis pulse - located on top of the foot (dorsalis pedis artery)
tibialis posterior pulse - located in the back of the ankle behind the medial malleolus (posterior tibial artery).
temporal pulse - located on the temple directly in front of the ear (temporal artery)
The ease of palpability of a pulse is dictated by the patient's blood pressure. If his or her systolic blood pressure is below 90 mmHg, the radial pulse will not be palpable. Below 80 mmHg, the brachial pulse will not be palpable. Below 60 mmHg, the carotid pulse will not be palpable. Since systolic blood pressure rarely drops that low, the lack of a carotid pulse usually indicates death. It is not unheard of, however, for patients with certain injuries, illnesses or other medical problems to be conscious and aware with no palpable pulse.
Heart disease is an umbrella term for a number of different diseases which affect the heart. The most common heart diseases are:
Coronary heart disease, a disease of the heart itself caused by the accumulation of atheromatous plaques within the walls of the arteries that supply the myocardium .
Ischaemic heart disease, another disease of the heart itself, characterized by reduced blood supply to the organ.
Cardiovascular disease, a sub-umbrella term for a number of diseases that affect the heart itself and/or the blood vessel system, especially the veins and arteries leading to and from the heart. Research on disease dimorphism suggests that women who suffer with cardiovascular disease usually suffer from forms that affect the blood vessels while men usually suffer from forms that affect the heart muscle itself. Known or associated causes of cardiovascular disease include diabetes mellitus, hypertension, hyperhomocysteinemia and hypercholesterolemia.
Pulmonary heart disease, a failure of the right side of the heart, not a good thing folks.
Hereditary heart disease, heart disease caused by unavoidable genetic factors since birth.
Hypertensive heart disease, heart disease caused by high blood pressure, especially localised high blood pressure .
Inflammatory heart disease, heart disease that involves inflammation of the heart muscle and/or the tissue surrounding it.
Valvular heart disease, heart disease that affects the valves of the heart.
Coronary Heart Disease
Coronary heart disease (CHD), also called coronary artery disease (CAD), ischaemic heart disease, and atherosclerotic heart disease, is the end result of the accumulation of atheromatous plaques within the walls of the arteries that supply the myocardium (the muscle of the heart). While the symptoms and signs of coronary heart disease are noted in the advanced state of disease, most individuals with coronary heart disease show no evidence of disease for decades as the disease progresses before the first onset of symptoms, often a "sudden" heart attack, finally arise. After decades of progression, some of these atheromatous plaques may rupture and (along with the activation of the blood clotting system) start limiting blood flow to the heart muscle. The disease is the most common cause of sudden death, and is also the most common reason for death of men and women over 65 years of age.
Atherosclerotic heart disease can be thought of as a wide spectrum of disease of the heart. At one end of the spectrum is the asymptomatic individual with atheromatous streaks within the walls of the coronary arteries (the arteries of the heart). These streaks represent the early stage of atherosclerotic heart disease and do not obstruct the flow of blood. A coronary angiogram performed during this stage of disease may not show any evidence of coronary artery disease, because the lumen of the coronary artery has not decreased in calibre.
Over a period of many years, these streaks increase in thickness. While the atheromatous plaques initially expand into the walls of the arteries, eventually they will expand into the lumen of the vessel, affecting the flow of blood through the arteries. While it was originally believed that the growth of atheromatous plaques was a slow, gradual process, recent evidence suggests that the gradual buildup of plaque may be complemented by small plaque ruptures which cause the sudden increase in the plaque burden due to accumulation of thrombus material. This is a common misconception many have had.
Atheromatous plaques that cause obstruction of less than 70 percent of the diameter of the vessel rarely cause symptoms of obstructive coronary artery disease. As the plaques grow in thickness and obstruct more than 70 percent of the diameter of the vessel, the individual develops symptoms of obstructive coronary artery disease. At this stage of the disease process, the patient can be said to have ischemic heart disease. The symptoms of ischemic heart disease are often first noted during times of increased workload of the heart. For instance, the first symptoms include exertional angina or decreased exercise tolerance.
As the degree of coronary artery disease progresses, there may be near-complete obstruction of the lumen of the coronary artery, severely restricting the flow of oxygen-carrying blood to the myocardium. Individuals with this degree of coronary heart disease typically have suffered from one or more myocardial infarctions (heart attacks), and may have signs and symptoms of chronic coronary ischemia, including symptoms of angina at rest and flash pulmonary edema.
A distinction should be made between myocardial ischemia and myocardial infarction. Ischemia means that the amount of oxygen supplied to the tissue is inadequate to supply the needs of the tissue. When the myocardium becomes ischemic, it does not function optimally. When large areas of the myocardium becomes ischemic, there can be impairment in the relaxation and contraction of the myocardium. If the blood flow to the tissue is improved, myocardial ischemia can be reversed. Infarction means that the tissue has undergone irreversible death due to lack of sufficient oxygen-rich blood.
An individual may develop a rupture of an atheromatous plaque at any stage of the spectrum of coronary heart disease. The acute rupture of a plaque may lead to an acute myocardial infarction (heart attack).
Blood Flow to Heart
Limitation of blood flow to the heart causes ischemia (cell starvation secondary to a lack of oxygen) of the myocardial cells. When myocardial cells die from lack of oxygen, this is called a myocardial infarction (commonly called a heart attack). It leads to heart muscle damage, heart muscle death and later scarring without heart muscle regrowth.
Myocardial infarction usually results from the sudden occlusion of a coronary artery when a plaque ruptures, activating the clotting system and atheroma-clot interaction fills the lumen of the artery to the point of sudden closure. The typical narrowing of the lumen of the heart artery before sudden closure is typically 20%, according to clinical research completed in the late 1990s and using IVUS examinations within 6 months prior to a heart attack. High grade stenoses as such exceeding 75% blockage, such as detected by stress testing, were found to be responsible for only 14% of acute heart attacks the rest being due to plaque rupture/ spasm. The events leading up to plaque rupture are only partially understood. Myocardial infarction is also caused, far less commonly, by spasm of the artery wall occluding the lumen, a condition also associated with atheromatous plaque and CHD.
CHD is associated with smoking, obesity, hypertension and a chronic sub-clinical lack of vitamin C. A family history of CHD is one of the strongest predictors of CHD. Screening for CHD includes evaluating homocysteine levels, high-density and low-density lipoprotein (cholesterol) levels and triglyceride levels.
Angina that occurs regularly with activity, upon awakening, or at other predictable times is termed stable angina and is associated with high grade narrowings of the heart arteries. The symptoms of angina are often treated with nitrate preparations such as nitroglycerin, which come in short-acting and long-acting forms, and may be administered transdermally, sublingually or orally. Many other more effective treatments, especially of the underlying atheromatous disease, have been developed.
Angina that changes in intensity, character or frequency is termed unstable. Unstable angina may precede myocardial infarction, and requires urgent medical attention. It is treated with morphine, oxygen, intravenous nitroglycerin, and aspirin. Interventional procedures such as angioplasty may be done.
Heart Disease Risk factors
The following are confirmed independent risk factors for the development of CAD, in order of decreasing importance:
*Hypercholesterolemia (specifically, serum LDL concentrations)
*Smoking
*Hypertension (high systolic pressure seems to be most significant in this regard)
* Hyperglycemia (due to diabetes mellitus or otherwise)
Hereditary differences in such diverse aspects as lipoprotein structure and that of their associated receptors, homocysteine processing/metabolism, etc.
Significant, but indirect risk factors include:
*Lack of exercise
*Stress
*Diet rich in saturated fats
*Diet low in antioxidants
*Obesity
*Men or Women over 65
Heart Disease Prevention
Coronary heart disease is the most common form of heart disease in the Western world. Prevention centers on the modifiable risk factors, which include decreasing cholesterol levels, addressing obesity and hypertension, avoiding a sedentary lifestyle, making healthy dietary choices, and stopping smoking. There is some evidence that lowering uric acid and homocysteine levels may contribute. In diabetes mellitus, there is little evidence that blood sugar control actually improves cardiac risk. Some recommend a diet rich in omega-3 fatty acids and vitamin C. The World Health Organization (WHO) recommends "low to moderate alcohol intake" to reduce risk of coronary heart disease.
An increasingly growing number of other physiological markers and homeostatic mechanisms are currently under scientific investigation. Among these markers are low density lipoprotein and asymmetric dimethylarginine. Patients with CHD and those trying to prevent CHD are advised to avoid fats that are readily oxidized (e.g., saturated fats and trans-fats), limit carbohydrates and processed sugars to reduce production of Low density lipoproteins while increasing High density lipoproteins, keeping blood pressure normal, exercise and stop smoking. These measures limit the progression of the disease. Recent studies have shown that dramatic reduction in LDL levels can cause mild regression of coronary heart disease.
Diet and Heart Disease
It has been suggested that coronary heart disease is partially reversible using an intense dietary regime coupled with regular cardio exercise.
Vegetarian diet: Vegetarians have been shown to have a 24% reduced risk of dying of heart disease.
Cretan Mediterranean-style diet: The Seven Country Study found that Cretan men had exceptionally low death rates from heart disease, despite moderate to high intake of fat. The Cretan diet is similar to other traditional Mediterranean diets: consisting mostly of olive oil, bread, abundant fruit and vegetables, a moderate amount of wine and fat-rich animal products such as lamb, sausage and goat cheese. However, the Cretan diet consisted of less fish and wine consumption than some other Mediterranean-style diets, such as the diet in Corfu, another region of Greece, which had higher death rates.
The consumption of trans fat (commonly found in hydrogenated products such as margarine) has been shown to cause the development of endothelial dysfunction, a precursor to atherosclerosis.
Aspirin can reduce the incidence of cardiovascular events. The U.S. Preventive Services Task Force 'strongly recommends that clinicians discuss aspirin chemoprevention with adults who are at increased risk for coronary heart disease'. The Task Force defines increased risk as 'Men older than 40 years of age, postmenopausal women, and younger persons with risk factors for coronary heart disease (for example, hypertension, diabetes, or smoking) are at increased risk for heart disease and may wish to consider aspirin therapy'. More specifically, high-risk persons are 'those with a 5-year risk ≥ 3%'. A risk calculator is available.
Regarding healthy premenopausal women, the more recent Women's Health Study randomized controlled trial found no insignficant benefit from aspirin in the reduction of cardiac events; however there was a signficant reduction in stroke. Subgroup analysis showed that all benefit was confined to women over 65 years old. In spite of the insignficant benefit for women < 65 years old, recent practice guidelines by the American Heart Association recommend to 'consider' aspirin in 'healthy women' <65 years of age 'when benefit for ischemic stroke prevention is likely to outweigh adverse effects of therapy'.
Secondary prevention is preventing further sequelae of already established disease. Regarding coronary heart disease, this can mean risk factor management that is carried out during cardiac rehabilitation, a 4-phase process beginning in hospital after MI, angioplasty or heart surgery and continuing for a minimum of three months. Exercise is a main component of cardiac rehabilitation along with diet, smoking cessation, and blood pressure and cholesterol management .
Cardiovascular Disease
Cardiovascular disease refers to the class of diseases that involve the heart and/or blood vessels (arteries and veins). While the term technically refers to any disease that affects the cardiovascular system, it is usually used to refer to those related to atherosclerosis (arterial disease).
These conditions have similar causes, mechanisms, and treatments. In practice, cardiovascular disease is treated by cardiologists, thoracic surgeons, vascular surgeons, neurologists, and interventional radiologists, depending on the organ system that is being treated. There is considerable overlap in the specialities, and it is common for certain procedures to be performed by different types of specialists in the same hospital.
Most Western countries face high and increasing rates of cardiovascular disease. Each year, heart disease kills more Americans than cancer. Diseases of the heart alone caused 30% of all deaths, with other diseases of the cardiovascular system causing substantial further death and disability. It is the number 1 cause of death and disability in the United States and most European countries. A large histological study (PDAY) showed vascular injury accumulates from adolescence, making primary prevention efforts necessary from childhood. By the time that heart problems are detected, the underlying cause (atherosclerosis) is usually quite advanced, having progressed for decades. There is therefore increased emphasis on preventing atherosclerosis by modifying risk factors, such as healthy eating, exercise and avoidance of smoking.
There are many risk factors which associate with (but are not all causes of) various forms of cardiovascular disease. These include the following:
*Age Gender, men under age 64 are much more likely to die of coronary heart disease than women, although the gender difference declines with age. (The gender difference is less pronounced in blacks than in whites, but it is still significant )
*Absence of key nutritional elements, such as omega-3 fats and polyphenol antioxidants
*Diabetes mellitus
*Hypercholesterolemia (elevated cholesterol levels) and abnormal lipoprotein particle profile (cholesterol subtypes)
*Elevated Heart Rate
*Tobacco smoking
*Higher fibrinogen and PAI-1 blood concentrations
*Elevated homocysteine, or even upper half of normal
*Elevated blood levels of asymmetric dimethylarginine
*High blood pressure
*Exposure to high levels of environmental noise
*Obesity, especially central or male-type obesity; apart from being linked to diabetes, this form of obesity independently increases cardiovascular risk, presumedly by inducing an inflammatory and procoagulant state
*Insulin resistance, especially when excess food calories are ingested
*Genetic factors/Family history of cardiovascular disease
*Physical inactivity/ Sedentary lifestyle
*Depression
*Stress
Although men have a higher rate of cardiovascular disease than women, it is also the number one health problem for women in industrialized countries. After menopause, the risk for women approaches that of men. Hormone replacement therapy alleviates a number of post-menopausal problems, but appears to increase the risk of cardiovascular disease.
Attempts to prevent cardiovascular disease are more effective when they remove and prevent causes, and they often take the form of modifying risk factors. Some factors, such as sex (male or female), age, and family history, cannot be modified. Smoking cessation (or abstinence) is one of the most effective and easily modifiable changes. Regular cardiovascular exercise (aerobic exercise) complements the healthful eating habits.
According to the American Heart Association, build up of plaque on the arteries (atherosclerosis), partly as a result of high cholesterol and fat diet, is a leading cause for cardiovascular diseases. The combination of healthy diet and exercise is a means to improve serum cholesterol levels and reduce risks of cardiovascular diseases; if not, a physician may prescribe "cholesterol-lowering" drugs, such as the statins. These medications have additional protective benefits aside from their lipoprotein profile improvement. Aspirin may also be prescribed, as it has been shown to decrease the clot formation that may lead to myocardial infarctions and strokes; it is routinely prescribed for patients with one or more cardiovascular risk factors.
One possible way to decrease risk of cardiovascular disease is keep your total cholesterol below 150. In the Framingham Heart Study, those with total cholesterol below 150 only very rarely got coronary heart disease.
Eating oily fish at least twice a week may help reduce the risk of sudden death and arrhythmias. A 2005 review of 97 clinical trials by Studer et al. noted that omega-3 fats gave lower risk ratios than did statins. Olive oil is said to have benefits. Studies of individual heart cells showed that fatty acids blocked excessive sodium and calcium currents in the heart, which could otherwise cause dangerous, unpredictable changes in its rhythm.
Interestingly, although cardiovascular is the number one cause of death for individuals in modern society, a majority of young people are unconcerned about their risk for development of this disease. Atherosclerosis is a process that develops over decades and is often silent until an acute event (heart attack) develops in later life. Population based studies in the youth show that the precursors of heart disease start in adolescence. The process of atherosclerosis evolves over decades, and begins as early as childhood. The Pathobiological Determinants of Atherosclerosis in Youth Study demonstrated that intimal lesions appear in all the aortas and more than half of the right coronary arteries of youths aged 15–19 years. However, most adolescents are more concerned about other risks such as HIV, accidents, and cancer than cardiovascular disease. This is extremely important considering that 1 in 3 people will die from complications attributable to atherosclerosis. In order to stem the tide of cardiovascular disease, primary prevention is needed. Primary prevention starts with education and awareness that cardiovascular disease poses the greatest threat and measures to prevent or reverse this disease must be taken.
Treatment of cardiovascular disease depends on the specific form of the disease in each patient, but effective treatment always includes preventive lifestyle changes discussed above. Medications, such as blood pressure reducing medications, aspirin and the statin cholesterol-lowering drugs may be helpful. In some circumstances, surgery or angioplasty may be warranted to reopen, repair, or replace damaged blood vessels.
The causes, prevention, and/or treatment of all forms of cardiovascular disease are active fields of biomedical research, with hundreds of scientific studies being published on a weekly basis. A fairly recent emphasis is on the link between low-grade inflammation that hallmarks atherosclerosis and its possible interventions. C-reactive protein (CRP) is an inflammatory marker that may be present in increased levels in the blood in patients at risk for cardiovascular disease. Its exact role in predicting disease is the subject of debate.
Some areas currently being researched include possible links between infection with Chlamydia pneumoniae and coronary artery disease. The Chlamydia link has become less plausible with the absence of improvement after antibiotic use .
Pulmonary heart disease - Cor pulmonale is a medical term used to describe a change in structure and function of the right ventricle of the heart as a result of a respiratory disorder. RVH (right ventricular hypertrophy) is the predominant change in chronic cor pulmonale, however in acute cases dilation dominates. Both hypertrophy and dilation are the result of increased right ventricular pressure. Dilation is essentially a stretching of the ventricle, the immediate result of increasing the pressure in an elastic container. Ventricular hypertrophy is an adaptive response to a long-term increase in pressure. Additional muscle grows to allow for the increased force in contraction required to move the blood against greater resistance. To be classified as cor pulmonale, the cause must originate in the pulmonary circulation. Vascular remodelling of the pulmonary circulation as a result of tissue damage (causes including disease, hypoxic injury, chemical agents, etc.) or chronic hypoxic vasoconstriction are two major causes. RVH due to a systemic defect is not classified as cor pulmonale. Left untreated, cor pulmonale can lead to right-heart failure and death.
Pulmonary heart diseaseTreatment - Elimination of the cause is the most important intervention. In pulmonary embolism, thrombolysis (enzymatic dissolution of the blood clot) is advocated if there is dysfunction of the right ventricle. In COPD, long-term oxygen therapy may improve cor pulmonale.
Cor pulmonale may lead to congestive heart failure (CHF), with worsening of respiration due to pulmonary edema, swelling of the legs due to peripheral edema and painful congestive hepatomegaly. This situation requires diuretics (to decrease strain on the heart), sometimes nitrates (to improve blood flow) and occasionally inotropes (to improve heart contractility). CHF is a negative prognostic indicator in cor pulmonale.
What is the Heart ?
The heart is a pear shaped, muscular organ in vertebrates, responsible for pumping blood through the blood vessels by repeated, rhythmic contractions, or a similar structure in annelids, mollusks, and arthropods. The term cardiac (as in cardiology) means "related to the heart" and comes from the Greek καρδία, kardia, for "heart." The heart is composed of cardiac muscle, an involuntary muscle tissue which is found only within this muscle.
The human embryonic heart begins beating approximately 21 days after conception, or five weeks after the last normal menstrual period (LMP), which is the date normally used to date pregnancy. The human heart begins beating at a rate near the mother’s, about 75-80 beats per minute (bpm). The embryonic heart rate (EHR) then accelerates linearly for the first month of beating, peaking at 165-185 bpm during the early 7th week, (early 9th week after the LMP). This acceleration is approximately 3.3 bpm per day, or about 10 bpm every three days, an increase of 100 bpm in the first month. There is no difference in male and female heart rates before birth
In the human body, the heart is normally situated to the left of the middle of the thorax, underneath the breastbone (see diagrams). The heart is usually felt to be on the left side because the left heart (left ventricle) is stronger (it pumps to all body parts). The left lung is smaller than the right lung because the heart occupies more of the left hemithorax. The heart is enclosed by a sac known as the pericardium and is surrounded by the lungs. The pericardium is a double membrane structure containing a serous fluid to reduce friction during heart contractions. The mediastinum, a subdivision of the thoracic cavity, is the name of the heart cavity.
The apex is the blunt point situated in an inferior (pointing down and left) direction. A stethoscope can be placed directly over the apex so that the beats can be counted. This physical location is between the sixth and seventh rib, just to the left of the sternum . In normal adults, the mass of the heart is 250-350 g (9-12 oz), or about three fourths the size of a clenched fist, but extremely diseased hearts can be up to 1000 g (2 lb) in mass due to hypertrophy. It consists of four chambers, the two upper atria (singular: atrium ) and the two lower ventricles. On the left is a picture of a fresh human heart which was removed from a 64-year-old British male.
The function of the right side of the heart (see right heart) is to collect deoxygenated blood, in the right atrium, from the body and pump it, via the right ventricle, into the lungs (pulmonary circulation) so that carbon dioxide can be dropped off and oxygen picked up (gas exchange). This happens through a passive process called diffusion. The left side (see left heart) collects oxygenated blood from the lungs into the left atrium. From the left atrium the blood moves to the left ventricle which pumps it out to the body. On both sides, the lower ventricles are thicker and stronger than the upper atria. The muscle wall surrounding the left ventricle is thicker than the wall surrounding the right ventricle due to the higher force needed to pump the blood through the systemic circulation.
If a person is encountered in cardiac arrest (no heartbeat), cardiopulmonary resuscitation (CPR) should be started, and help called. If an automated external defibrillator is available, this device may automatically administer defibrillation if this is indicated.
Heart cancer is an extremely rare form of cancer of the heart. Heart cancer is divided into primary tumors of the heart and secondary tumors of the heart. Most heart cancers are benign myxomas, fibromas, rhabdomyomas and hamartomas, although malignant sarcomas (such as angiosarcoma or cardiac sarcoma) have been known to occur. In a study of 12,487 autopsies performed in Hong Kong seven cardiac tumors were found, most of which were benign. However, cancer can also spread to heart from other parts of the body. In addition the heart can be affected by treatment for cancer in other parts of the body
A congenital heart defect (CHD) is a defect in the structure of the heart and great vessels of the newborn. Most heart defects either obstruct blood flow in the heart or vessels near it or cause blood to flow through the heart in an abnormal pattern, although other defects affecting heart rhythm (such as long QT syndrome) can also occur. Heart defects are among the most common birth defects, and are the leading cause of birth defect-related deaths.
Slightly less than 1% of all newborn infants have congenital heart disease. Eight defects are more common than all others and make up 80% of all congenital heart diseases, whereas the remaining 20% consist of many independently infrequent conditions or combinations of several defects. Ventricular septal defect (VSD) is generally considered to be the most common type of malformation, accounting for about 1/3 of all congenital heart defects.
The incidence is higher when a parent or a sibling has a heart defect (4-5%), in stillborns (3-4%), abortuses (10-25%), and premature infants (2%).
The number of adults with problems connected to a congenital heart defect is rising and is passing the number of children with congenital heart defects in most western countries. This group is called GUCH patients.
The cause of most congenital heart defects is unknown. Where a cause is known, it may be of a multifactorial origin and/or a result of genetic predisposition and environmental factors. Known genetic causes of heart disease includes chromosomal abnormalities such as trisomies 21, 13, and 18, as well as a range of newly recognised genetic point mutations, point deletions and other genetic abnormalities as seen in syndromes such as CATCH 22, familial ASD with heart block, Alagille syndrome, Noonan syndrome, and many more.
Known antenatal environmental factors include maternal infections (Rubella), drugs (alcohol, hydantoin, lithium and thalidomide) and maternal illness (diabetes mellitus, phenylketonuria, and systemic lupus erythematosus).
Symptoms and signs are related to the type and severity of the heart defects. Some children have no signs while others may exhibit shortness of breath, cyanosis, chest pain, syncope, sweating, heart murmur, respiratory infections, underdeveloping of limbs and muscles, poor feeding, or poor growth. Most defects cause a whispering sound, or murmur, as blood moves through the heart causing some of these symptoms. All of these symptoms occur at a young age of a child or infant which is typically found during a physical examination.
Heart rate is a term used to describe the frequency of the cardiac cycle. It is considered one of the four vital signs. Usually it is calculated as the number of contractions (heart beats) of the heart in one minute and expressed as "beats per minute" (bpm). See "Heart" for information on embryofetal heart rates. The heart beats up to 120 times per minute in childhood. When resting, the adult human heart beats at about 70 bpm (males) and 75 bpm (females), but this rate varies among people. However, the resting heart rate can be significantly lower in athletes. The infant/neonatal rate of heartbeat is around 130-150 bpm, the toddler's about 100–130 bpm, the older child's about 90–110 bpm, and the adolescent's about 80–100 bpm.
The pulse is the most straightforward way of measuring the heart rate, but it can be deceptive when some heart beats do not have much cardiac output. In these cases (as happens in some arrhythmias), the heart rate may be considerably higher than the pulse rate. Auscultation is also a method of heart rate measurement.
The heart contains two cardiac pacemakers that spontaneously cause the heart to beat. These can be controlled by the autonomic nervous system and circulating adrenaline. The vagus nerve (which is pneumogastric nerve or cranial nerve X) which governs heart rate can be controlled through breathing.
Measuring heart rate - The pulse rate (which in most people is identical to the heart rate) can be measured at any point on the body where an artery is close to the surface. Such places are wrist (radial artery), neck (carotid artery), elbow (brachial artery), and groin (femoral artery). The pulse can also be felt directly over the heart. NOTE: The thumb should never be used for measuring heart rate. Producing an electrocardiogram, or ECG (also abbreviated EKG), is one of the most precise methods of heart rate measurement. Continuous electrocardiographic monitoring of the heart is routinely done in many clinical settings, especially in critical care medicine. Commercial heart rate monitors are also available, consisting of a chest strap with electrodes. The signal is transmitted to a wrist receiver for display. Heart rate monitors allow accurate measurements to be taken continuously and can be used during exercise when manual measurement would be difficult or impossible (such as when the hands are being used). It is also common to find heart rate by listening, via a stethoscope, to the movement created by the heart as it contracts within the chest
Heart rate variability (HRV) is the variation of beat-to-beat intervals. A healthy heart has a large HRV, while decreased or absent variability may indicate cardiac disease. HRV also decreases with exercise-induced tachycardia. HRV has been the focus of increased research to use it as a physiological marker to classify different pathological disorders.
One aspect of heart rate variability can be used as a measurement of fitness, specifically the speed at which one's heart rate drops upon termination of vigorous exercise. The speed at which a person's heart rate returns to resting is considerably faster for a fit person than an unfit person. A drop of 20 beats in a minute is typical for a healthy person. A drop of less than 12 beats per minute after maximal exercise has been correlated with a significant increase in mortality
Maximum heart rate (also called MHR, or HRmax) is the maximum heart rate that a person should achieve during maximal physical exertion. Research indicates it is most closely linked to a person's age; a person's HRmax will decline as they age. Some research indicates the speed at which it declines over time is related to fitness—the more fit a person is, the more slowly it declines as they age.
HRmax is utilized frequently in the fitness industry, specifically during the calculation of target heart rate when prescribing a fitness regimen. A quick way to estimate MHR is to subtract your age from 220, but HRmax can vary significantly between same-aged individuals so direct measurement using a heart rate monitor (and with medical supervision or at least permission and advice) should be used by those seeking maximum safety and effectiveness in their training. People who have participated in sports and athletic activities in early years will have a higher MR than those less active as children.
Training Heart rates - (Warm up) — 50–60% of maximum heart rate: The easiest zone and probably the best zone for people just starting a fitness program. It can also be used as a warm up for more serious walkers. This zone has been shown to help decrease body fat, blood pressure and cholesterol. It also decreases the risk of degenerative diseases and has a low risk of injury. Fats are 85% of food energy burned in this zone.
Fitness Zone (Fat Burning) — 60–70% of maximum heart rate: This zone provides the same benefits as the healthy heart zone, but is more intense and burns more total food energy. The percent of food energy from fat is still 85%.
Aerobic Zone (Endurance Training) — 70–80% of maximum heart rate: The aerobic zone will improve your cardiovascular and respiratory system and increase the size and strength of your heart. This is the preferred zone if you are training for an endurance event. More food energy is burned with 50% from fat.
Anaerobic Zone (Performance Training) — 80–90% of maximum heart rate: Benefits of this zone include an improved FPRIVATE "TYPE=PICT;ALT=V_{\mathrm{O}_2 }" maximum (the highest amount of oxygen one can consume during exercise) and thus an improved cardio-respiratory system, and a higher lactate tolerance ability which means your endurance will improve and you'll be able to fight fatigue better. This is a high intensity zone burning more food energy, 15% from fat.
Red Line (Maximum Effort) — 90–100% of maximum heart rate: Although this zone burns the highest amount of food energy, it is very intense. Most people can only stay in this zone for short periods. You should only train in this zone if you have a very high fitness level and have been cleared by a physician to do so.
Recovery heart rate - The recovery heart rate is one that is taken several minutes after exercise. It is taken anywhere between 2–10 minutes after exercise. It is taken for 15 seconds, and is multiplied by four in order to calculate beats per minute (bpm). The goal is not to exceed 120 bpm.
Target heart rate (THR), or training heart rate, is a desired range of heart rate reached during aerobic exercise which enables one's heart and lungs to receive the most benefit from a workout. This theoretical range varies based on one's physical condition, age, and previous training. Below are two ways to calculate one's Target Heart Rate. In each of these methods, there is an element called "intensity" which is expressed as a percentage. THR can be calculated by using a range of 50%–85% intensity.
Heart rate reserve (HRR) is a term used to describe the difference between a person's maximum heart rate and predicted heart rate (or actual heart rate). Some methods of measurement of exercise intensity measure percentage of heart rate reserve. Additionally, as a person increases their cardiovascular fitness, their HRrest will drop, thus the heart rate reserve will increase. Percentage of HRR is equivalent to percentage of VO2reserve.
Heart rate abnormalities :
Tachycardia is a resting heart rate more than 100 beats per minute. This number can vary as smaller people and children have faster heart rates than adults.
Bradycardia is defined as a heart rate less than 60 beats per minute although it is seldom symptomatic until below 50 bpm. Trained athletes tend to have slow resting heart rates, and resting bradycardia in athletes should not be considered abnormal if the individual has no symptoms associated with it. Again, this number can vary as smaller people and children have faster heart rates than adults
In medicine, a person's pulse is the throbbing of their arteries as an effect of the heart beat. It can be felt at the neck, at the wrist and other places.
Pressure waves move through the blood vessels, which are pliable; these waves are not caused by the forward movement of the blood. When the heart contracts, blood is ejected into the aorta and the aorta stretches. At this point the wave of distention (pulse wave) is pronounced but relatively slow-moving (3 to 6 m/s). As it travels towards the peripheral blood vessels, it gradually diminishes and becomes faster. In the large arterial branches, its velocity is 7 to 10 m/s; in the small arteries, it is 15 to 35 m/s. The pressure pulse is transmitted 15 or more times more rapidly than the blood flow.
The term pulse is also used, although incorrectly, to denote the frequency of the heart beat, usually measured in beats per minute. In most people, the pulse is an accurate measure of heart rate. Under certain circumstances, including arrhythmias, some of the heart beats are ineffective and the aorta is not stretched enough to create a palpable pressure wave. The pulse is irregular and the heart rate can be (much) higher than the pulse rate. In this case, the heart rate should be determined by auscultation of the heart apex, in which case it is not the pulse. The pulse deficit (difference between heart beats and pulsations at the periphery) should be determined by simultaneous palpation at the radial artery and auscultation at the heart apex.
A normal pulse rate for a healthy adult, while resting, can range from 60 to 100 beats per minute (BPM). During sleep, this can drop to as low as 40 BPM; during strenuous exercise, it can rise as high as 200–220 BPM. Generally, pulse rates are higher in younger persons. A resting heart rate for an infant is as high as or higher than an adult's pulse rate during strenuous exercise.
Besides its rate, the pulse has other qualities which reflect the state of the cardiovascular system, such as its rhythm, fullness and the shape of the pulse wave. Certain diseases cause characteristic changes in these qualities. The absence of a pulse at the temple of the skull can be a sign of giant cell arteritis; absent or decreased pulses in the limbs may indicate peripheral artery occlusive disease.
Pulses are manually palpated with fingers or thumb. When palpating the carotid artery, the femoral artery or the brachial artery, the thumb may be used. However, the thumb has its own pulse which can interfere with detecting the patient's pulse at other points, where two or three fingers should be used. Fingers or thumb must be placed near an artery and pressed gently against a firm structure, usually a bone, in order to feel the pulse.
An alternative way of finding the pulse rate is by palpating or listening to the heartbeat. This is most commonly done with the examiner's palm or a through a stethoscope. Before the invention of the stethoscope examiners would press their ear directly to the chest.
Common pulse points :
radial pulse - located on the thumb side of the wrist (radial artery)
ulnar pulse - located on the little finger side of the wrist (ulnar artery)
carotid pulse - located in the neck (carotid artery). The carotid artery should be palpated gently. Stimulating its baroreceptors with vigorous palpitation can provoke severe bradycardia or even stop the heart in some sensitive persons. Also, a person's two carotid arteries should not be palpated at the same time, to avoid a risk of fainting or brain ischemia.
brachial pulse - located between the biceps and triceps, on the medial side of the elbow cavity; frequently used in place of carotid pulse in infants (brachial artery)
femoral pulse - located in the thigh (femoral artery)
popliteal pulse - located behind the knee in the popliteal fossa, found by holding the bent knee. The patient bends the knee at approximately 120°, and the physician holds it in both hands to find the popliteal artery in the pit behind the knee.
dorsalis pedis pulse - located on top of the foot (dorsalis pedis artery)
tibialis posterior pulse - located in the back of the ankle behind the medial malleolus (posterior tibial artery).
temporal pulse - located on the temple directly in front of the ear (temporal artery)
The ease of palpability of a pulse is dictated by the patient's blood pressure. If his or her systolic blood pressure is below 90 mmHg, the radial pulse will not be palpable. Below 80 mmHg, the brachial pulse will not be palpable. Below 60 mmHg, the carotid pulse will not be palpable. Since systolic blood pressure rarely drops that low, the lack of a carotid pulse usually indicates death. It is not unheard of, however, for patients with certain injuries, illnesses or other medical problems to be conscious and aware with no palpable pulse.
